What it takes to diagnose the disease
Guidelines that can help diagnose iMCD
The Castleman Disease Collaborative Network (CDCN) convened a working group of 34 international
experts that established the first evidence-based consensus treatment guidelines for
iMCD, based on a review of 244 cases and 88 tissue samples. Below are some highlights
from the CDCN guidelines that can help achieve an accurate diagnosis.1
Major Criteria
(need both)

Histology consistent with Castelman disease (CD)
≥2 enlarged lymph node groups
Minor Criteria (need ≥2, with ≥1 laboratory criterion)

Clinical abnormality
- Constitutional symptoms
- Large spleen and/or liver
- Fluid accumulation
- Violaceous papules
- Lymphocytic Interstitial pneumonitis

Laboratory abnormality
- Elevated CRP
- Anemia
- Thrombocytopenia
- Hypergammaglobulinemia
- Hypoalbuminemia
- Renal dysfunction
Exclusion Criteria

Exclude diseases that iMCD can mimic, such as autoimmune, malignant and infectious diseases.
In order to diagnose a patient with iMCD, you must ensure they meet both Major Criteria and at
least 2 of the 11 Minor Criteria, including ≥1 laboratory abnormality, and rule out diseases in
the Exclusion Criteria1
You can download a detailed, print-ready version of the CDCN Diagnostic Criteria, which includes a checklist that can help you during the diagnostic process.
Key workup to facilitate the differential diagnosis of iMCD
Additionally, tests must be performed to exclude diseases that can mimic iMCD, HHV-8, or human
immunodeficiency virus (HIV) infection.1
Excisional biopsy ensures pathologic confirmation of iMCD
Fine-needle aspiration or core biopsy is unlikely to capture the affected tissue within the lymph node and may be inadequate to get an accurate diagnosis of iMCD.2-4
An excisional biopsy enables a pathologist to conduct the complete examination of the total lymph node architecture.2,5
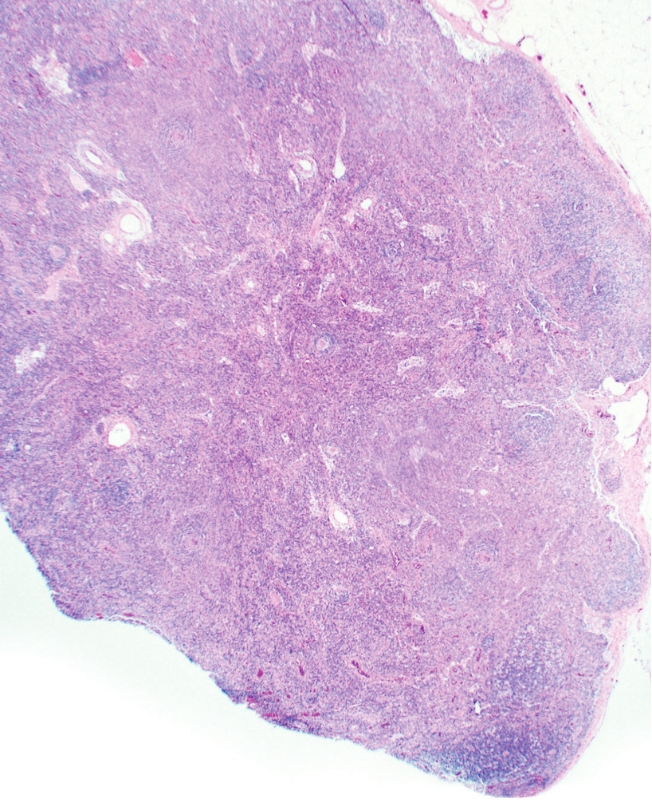
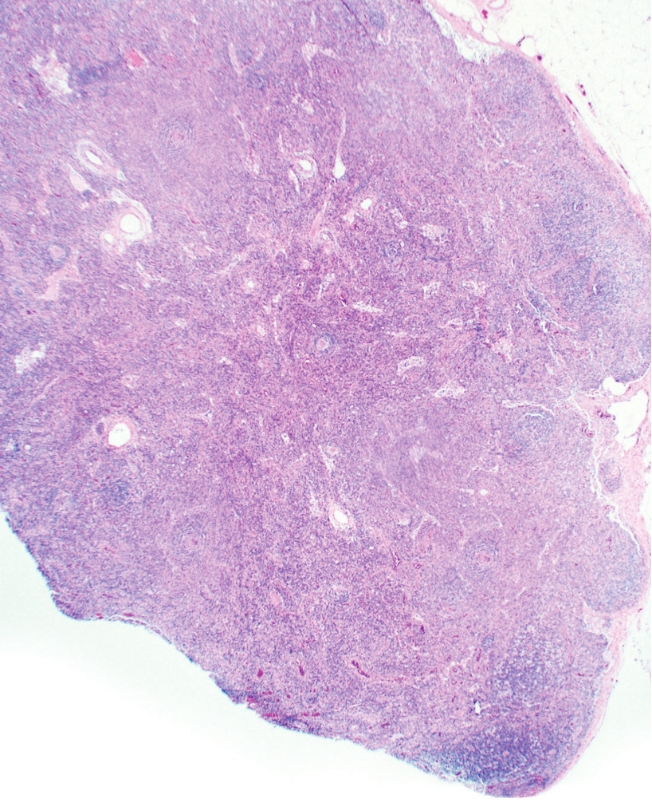
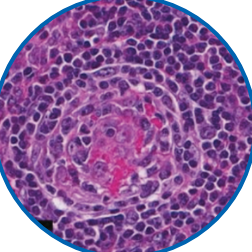
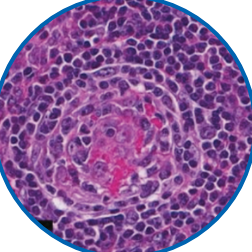
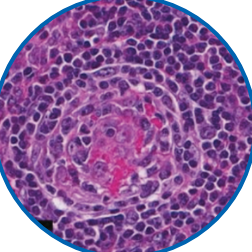
Jadee L. Neff, MD, PhDIf you have a patient who has unexplained lymphadenopathy, unexplained constitutional symptoms, and they can’t seem to get to a diagnosis, I would recommend an excisional biopsy [to] get a complete look at the lymph node.

Sign up for more on iMCD
"*" indicates required fields
By checking the adjacent box, you agree to allow EUSA Pharma to collect the information provided and to be contacted by EUSA Pharma in the future regarding its IL-6 neutralizing products and related disease education.
By submitting this form, you agree to allow EUSA Pharma to collect the information provided and to be contacted directly by a EUSA Pharma sales representative. Your information will not be used for any other purpose than for a representative to respond to your information request, or for us to send you other EUSA Pharma updates if you have registered to receive them.
EUSA Pharma will not sell, rent, or otherwise distribute your name and any personally identifiable information outside of EUSA Pharma. EUSA Pharma will only use your information in accordance with its Privacy Policy.
-
Fajgenbaum DC, Uldrick TS, Bagg A, et al. International, evidence-based consensus diagnostic criteria for HHV-8–negative/idiopathic multicentric Castleman disease. Blood. 2017;129(12):1646-1657.
-
Allin D, David S, Jacob A, Mir N, Giles A, Gibbins N. Use of core biopsy in diagnosing cervical lymphadenopathy: a viable alternative to surgical excisional biopsy of lymph nodes? Ann R Coll Surg Engl. 2017;99(3):242-244.
-
Gaurin GE, da Costa Dourado CM. Castleman disease. Medscape. https://emedicine.medscape.com/article/2219018-overview. Updated November 24, 2021. Accessed April 21, 2022.
-
Early detection, diagnosis, and staging of Castleman disease. American Cancer Society. https://www.cancer.org/content/dam/CRC/PDF/Public/8596.00.pdf. Revised February 8, 2018. Accessed May 11, 2022.
-
van Rhee F, Voorhees P, Dispenzieri A, et al. International, evidence-based consensus treatment guidelines for idiopathic multicentric Castleman disease. Blood. 2018;132(20):2115-2124.
-
Mahmud SA, Binstadt BA. Autoantibodies in the pathogenesis, diagnosis, and prognosis of juvenile idiopathic arthritis. Front Immunol. 2019;9:3168.
-
Autoimmune condition. National Cancer Institute. https://www.cancer.gov/publications/dictionaries/cancer-terms/def/autoimmune-condition. Accessed June 9, 2022.
-
Shanbhag S, Ambinder RF. Hodgkin lymphoma: a review and update on recent progress. CA Cancer J Clin. 2018;68(2):116-132.
-
Cheson BD, Fisher RI, Barrington SF, et al. Recommendations for initial evaluation, staging, and response assessment of Hodgkin and non-Hodgkin lymphoma: the Lugano classification. J Clin Oncol. 2014;32(27):3059-3067.
-
Fugl A, Andersen CL. Epstein-Barr virus and its association with disease - a review of relevance to general practice. BMC Fam Pract. 2019;20(1):62.
-
Mononucleosis: symptoms and causes. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/mononucleosis/symptoms-causes/syc-20350328. Published December 22, 2020. Accessed June 9, 2022.
-
HIV/AIDS: symptoms and causes. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/hiv-aids/symptoms-causes/syc-20373524. Published February 13, 2020. Accessed June 9, 2022.
Your iMCD Diary
Save and use this Patient Diary online with your Google account by selecting “Google Sheet” and then “Use Template,” or download to your computer by selecting “Excel File.”
No data is stored by or transferred to this KnowiMCD.com website. This site contains links to other websites, and these links will direct users to third-party sites.
Loading...
Please wait a moment.
Are you located in the United States?
If so, you will be directed to the website that contains information intended for a US audience.
Viral hemophagocytic lymphohistiocytosis.
A doctor who specializes in the branch of medicine that deals with rheumatic conditions.
Polyneuropathy, organomegaly, endocrinopathy, monoclonal gammopathy, and skin changes.
Positron emission tomography (PET) is a method of producing a 3-dimensional image of the internal
structures of body tissues after administering a natural biochemical substance like glucose or fatty
acids. These images are generated with the help of a computer.
A doctor who evaluates the changes caused by disease in tissues and body fluids and helps reach a
diagnosis.
A doctor who specializes in the diagnosis and treatment of kidney abnormalities.
Macrophage activation syndrome.
Malignancy-associated hemophagocytic lymphohistiocytosis.
A disease in which cells of the lymph system grow excessively
Lymph nodes make immune cells that help the body fight infection.
A key signaling molecule that helps to regulate the body’s immune system.
Infectious disease medicine is the subspecialty of internal medicine that focuses on diagnosing and
managing infections.
A rare condition that affects multiple groups of lymph nodes throughout the body. Patients with iMCD
are HIV negative and HHV-8 negative.
The underlying cause or origin of a disease is unknown.
Hemophagocytic lymphohistiocytosis.
Human immunodeficiency virus.
Human herpesvirus-8.
A doctor who specializes in the branch of medical science that deals with cancers of the blood and
blood-forming tissues.
Powerful molecules that are normally secreted by the cells of the immune system in response to
infectious or noninfectious agents.
An overreaction of the body’s immune system in which too many cytokines are released into the
bloodstream very quickly, with potentially severe or life-threatening effects.
Computed tomography (CT) is a method of producing an image of the internal structures by passing an
x‑ray through the body.
The removal and examination of tissue, cells, or fluids from the body.
A condition in which the body’s immune system accidentally attacks itself.
Autoimmune lymphoproliferative syndrome.
You are now leaving KnowiMCD.com.
Please click “OK” to continue or “CANCEL” to return to KnowiMCD.com
